Brucellosis – Mediterranean Fever
Brucellosis is a infectious bacterial disease caused by various Brucella species. Animals are the most commonly infected include sheep, cattle, goats, swine, pigs, and dogs and infection transmitted from animals to people.
Humans become infected with brucellosis disease through direct contact with infected animals, or by ingesting and drinking contaminated animal products or by breathe airborne agents with the bacteria. People mostly get infection by consuming unpasteurized dairy products.
Epidemiological Triad
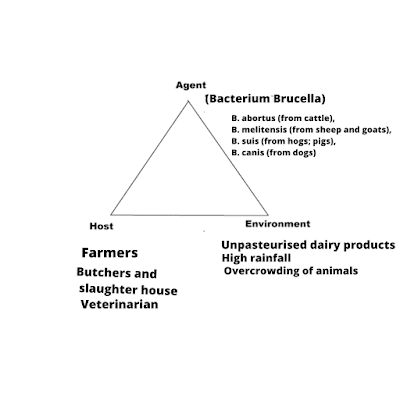
Agent – Brucellosis is caused by Brucella melitensis, Brucella abortus, Brucella suis, Brucella canis, in the family Brucellaceae.
Host – People, who are at high risk are- Butchers, Farmers, Veterinarians, Shepherds, Laboratory workers.
Environment – High rain fall, Overcrowding of herds,
Unhygienic milk and meat production practices, Organisms favourable condition to survive, Lack of exposure to sunlight, Conditions of water, urine, faeces and manure (animal dung)
Mode of Transmission
Infected animals to Man
1. By consuming unpasteurized/raw dairy products or eating undercooked meat
The most common way to be infected is by ingesting, drinking unpasteurized and raw dairy products. When animals such as sheep, goats, cows, or camels are infected with Brucellosis, then their milk contaminated with the bacterial infection.
The infection will be spread to human by consuming the infected milk and/or dairy products, if the infected animals milk is not pasteurized.
2. Direct Contact – Direct contact with infected animal tissue, blood, urine or vaginal discharge of abraded skin, mucosa or conjunctiva.
3. Inhalation in the bacteria that cause brucellosis (Air Borne; Breathing)
Breathing in the bacterial contaminated environment can causes brucellosis and lead to infection. By Inhalation dust of aerosols containing infection of Brucella.
Those people in laboratories work with the bacteria are generally risk of infection increases.
Slaughterhouse worker and meat-packing employees also exposed to the bacteria and becoming infected.
4. Bacteria entering the body through skin wounds or mucus membranes
Bacteria can also enter wounds in the skin or mucous membranes through contact with infected animals.
Thoseworkers such as slaughterhouse workers, farmers, butchers, meat-packing plant employees, hunters, veterinarian, laboratory personnel come in close contact with animals or animal excretions (newborn animals, foetuses, and excretions; result from birth) increase chance to expose to the bacteria.
5. Food borne – Becoming infected of eating of raw material or dairy products from infected animals or eating of fresh raw vegetable grown in contaminated soil can infect and cause brucellosis.
6. Transmission human to human infection of brucellosis infection is extremely rare. Infected mothers may transmit infection to their infants by breastfeeding.
Incubation Period
The incubation period of the disease can be varying, ranging from 1 week to 2 months, but usually – 4 weeks.
Clinical Manifestation
Initial symptoms of brucellosis can include-
1. Fever, Sweats
2. Malaise
3. Anorexia
4. Headache
5. Pain in muscles, joint, Low Back pain
6. Fatigue
7. Headache
8. Insomnia
Some signs and symptoms may persist for longer periods of time, include-
1. Recurrent fevers, Intermittent or irregular fever or swinging pyrexia (103°F – 104°F)
2. Profuse sweating, rigors
3. Arthritis – Involves larger joints
3. Swelling of the testicle and scrotum area
4. Swelling of the heart (endocarditis)
5. Neurologic symptoms (in up to 5% of all cases)
6. Chronic fatigue
7. Enlargement of the liver and/or spleen; Hepatomegaly, Splenomegaly
Laboratory Diagnosis
Isolating organism from culture of a. Blood, b. Bone marrow, c. other body fluids
1. Testing blood for the brucella bacteria
2. Bone marrow testing for the brucella bacteria
3. Testing blood for antibodies to the bacteria
4. X-rays – To help detect complications of brucellosis, X-rays can reveal changes in your bones and joints
5. Brucella microagglutination test (BMAT); modified version of the serum (tube) agglutination test (SAT) – To detect antibodies to Brucella species -B. abortus, B. melitensis, B. suis.
To detect antibodies for the bacteria Brucella Canis, there is no serological test available.
Risk of Exposure
1. Contaminated environment – Areas at Risk
2. Occupational Risks
People are in certain occupations or settings can increase exposure to the bacteria and cause brucellosis.
The occupation such as – Slaughterhouse workers, meat-packing employees, veterinarians, laboratory workers, cowherd, butchers.
3. Hunters Risks
Many animals may infect with brucellosis disease. Hunter may be increased risk of brucellosis, if hunt infected animal, because of may come into contact with their blood and organs of the animals.
Hunter gets illness if blood, fluid, or tissue from an infected animal comes in contact with skin wound , eyes, nose, mouth.
4. Risks for Expecting Mothers
Pregnant women who exposed to brucellosis recommended laboratory tests and prescribed short course of antibiotics, known as post-exposure prophylaxis (PEP). Prompt diagnosis and treatment of brucellosis during pregnancy, can lifesaving for the fetus.
Treatment of Brucellosis
Cases of Brucellosis treated with antibiotics. Before the treatment, diagnosis should be done for brucellosis infection.
Treatment options for brucellosis infection include- Doxycycline, Streptomycin, Tetracycline, Rifampicin, Gentamicin.
Prevention and Control of Brucellosis
1. Early diagnosis and treatment
2. Boiling/Pasteurisation of milk
Pasteurize of milk before consumption. It destroys and kill harmful pathogens that make milk to safe to consume.
3. Prevent from Direct contact to suspected animals
4. Measure the food safety
Don’t consume raw or undercooked meat.
5. Vaccination – For the humans, who are at risk.
Vaccines are recommended to control the disease in animals; cattle, goats and sheep.
6. Personal hygiene and Hygiene of Environment
In agricultural work and meat-processing industry, wear protective barriers and correct handling of animal, disposal of after births, placenta, blood product, animal carcasses and internal organs is an must be done.
7. Testing the animals
8. Occupational hygiene and laboratory safety
People who handle animal tissues must protect themselves by using – Rubber gloves, Goggles, Gowns or aprons to prevent from bacteria from infected animals, get into eyes, mouth or inside a cut or abrasion on the skin.
Brucellosis Question And Answer
1. What is brucellosis?
Brucellosis is a bacterial infectious disease caused by various Brucella species; Brucella melitensis, Brucella abortus, Brucella suis, Brucella canis, in the family Brucellaceae.
2. What are the causes of brucellosis?
Animals are the most commonly infected with brucellosis infection includes sheep, cattle, goats, swine, pigs, and dogs. The infection transmitted from animals to people through direct contact with infected animals, by ingesting or drinking contaminated animal products or by inhaling airborne agents with the bacteria.
3. How is brucellosis transmitted?
Bacteria Brucella spread by –
Consuming unpasteurized or raw dairy products or eating , Eating raw or undercooked meat or direct contact of abraded skin, mucosa or conjunctiva with infected animal tissue, blood, urine or vaginal discharge.
4. What is the treatment of brucellosis?
Brucellosis infection treated with antibiotics. Antibiotic Treatment options include Doxycycline , Tetracycline, Streptomycin, Rifampicin, Gentamicin.
Consuming unpasteurized milk may also cause Salmonellosis infection, Know the sign and symptoms of a salmonellosis.


